Deciding on what to do after you experience HG is a very difficult question. Knowing HG recurs in over 75% of women means you have to be prepared to go through it again. Being prepared with a doctor and support network is crucial to survival. These questions should help you and your partner make these important decisions.
If you have had HG more than once, you have a very high probability of having HG again. Recent research by the HER Foundation finds over half of women (about 2/3rds) will have HG in every pregnancy. Your chances are greater if you have a relative with a history of HG, especially a sister. Health professionals often underestimate the recurrence rate of HG. HG is not necessarily a sign that something is wrong in your pregnancy, so terminating and trying again is not a strategy to avoid HG.
Don't assume your next pregnancy will be different. Subsequent pregnancies are often similar though sometimes they vary - either better or worse. For some women, each pregnancy gets more severe, others know more how to prepare and cope so ultimately it feels less severe. Knowing how to manage it better makes future pregnancies somewhat easier. Hope for the best, but always be very prepared for the worst.
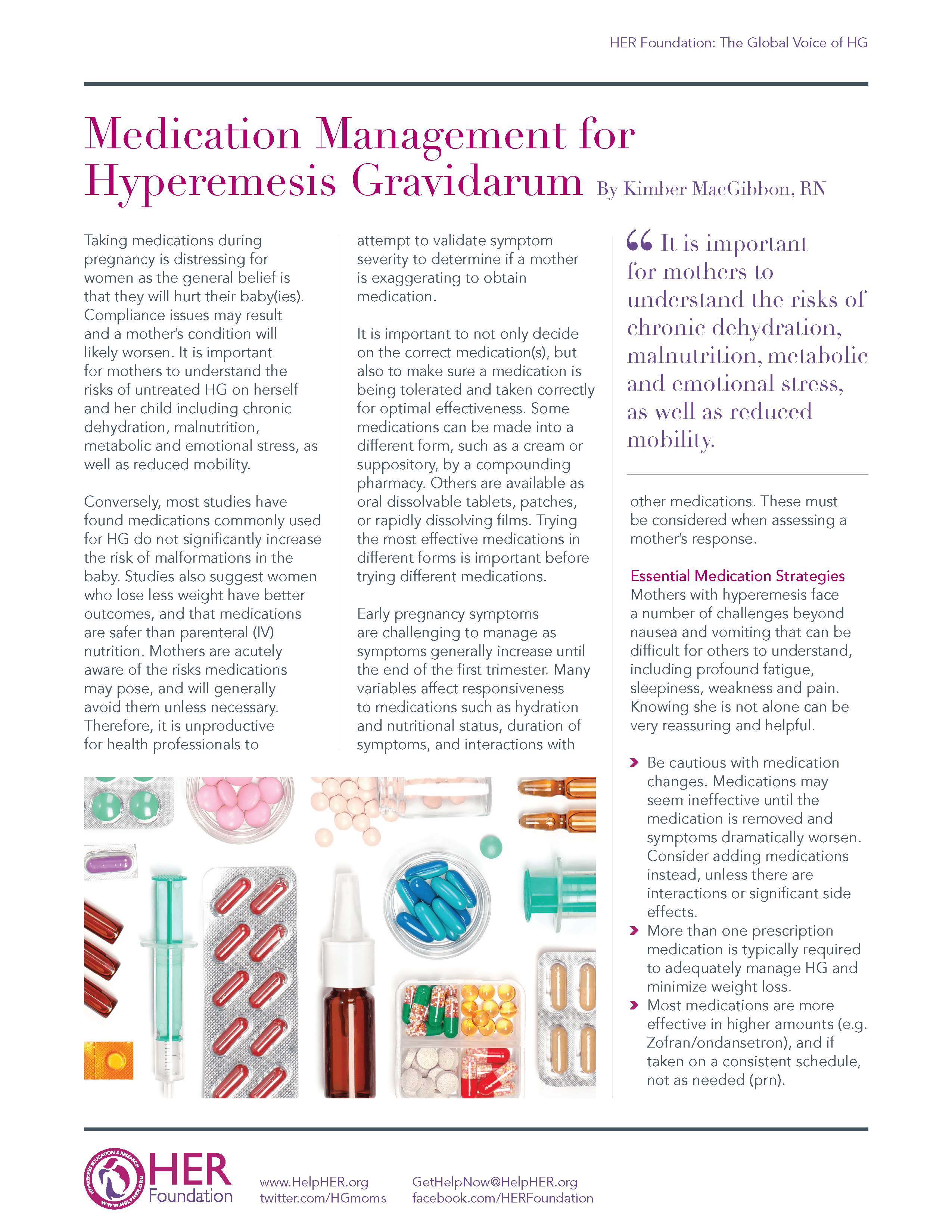
If yes, and they did not work, know that there are few other options available currently, and you may be limited to those treatment options. Do understand that few medications target nausea directly because it's mechanisms are not fully understood. So if your medications reduced the vomiting, they were working.
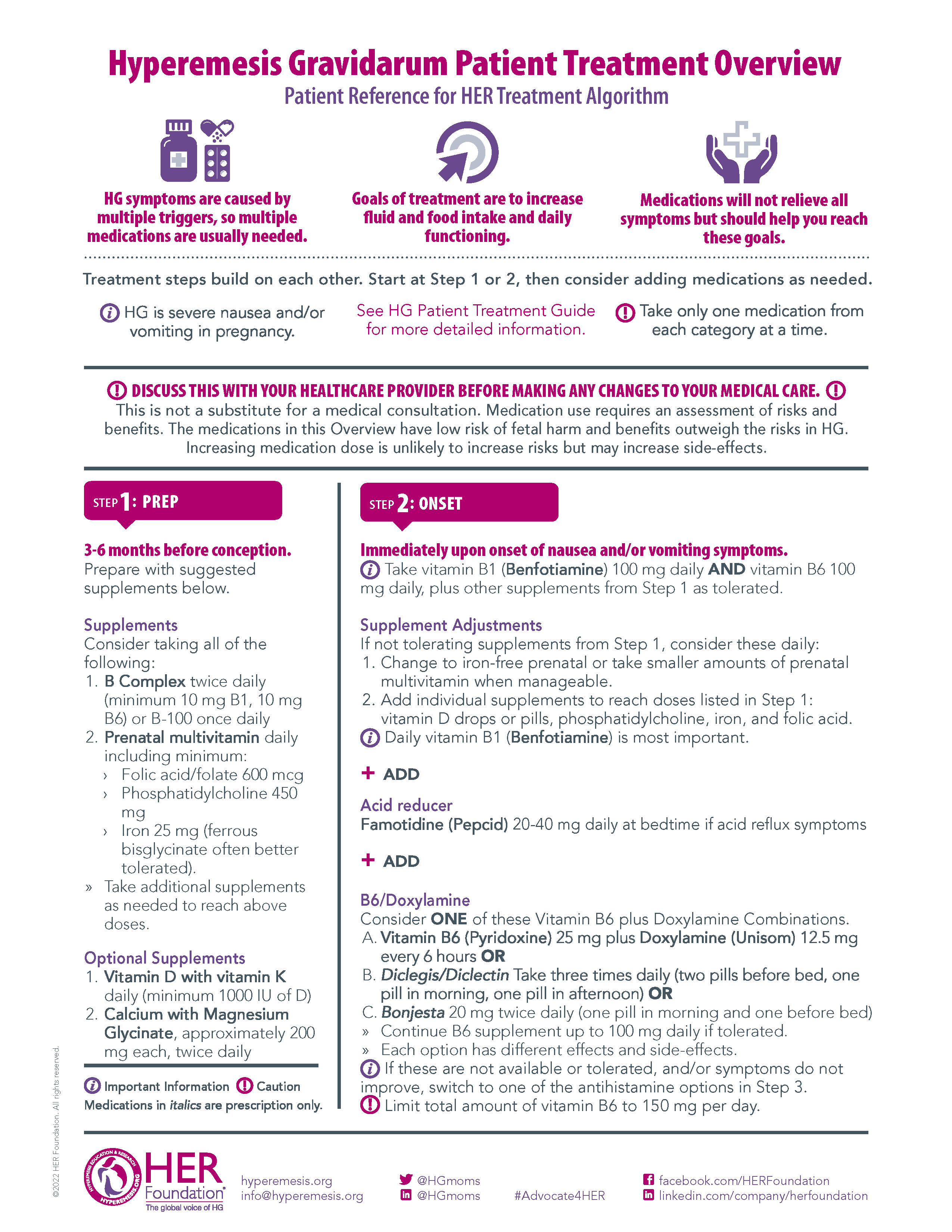
For some women, starting treatment earlier in pregnancy - at the onset of HG rather than after symptoms are severe, makes surviving HG possible. Getting IV vitamins during pregnancy and taking high quality B vitamins and prenatals prior to pregnancy may help reduce symptoms.
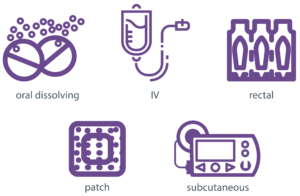
Also, for some, getting medications via a patch, compounded into a suppository or cream, or by an IV or subcutaneous pump that offers continuous dosing, may be very beneficial.
For a small number of women, treatments are not tolerated or have limited beneficial effect in any combination. Aggressive care with nutritional intervention and multiple medications at the start of symptoms is likely the best strategy. These women often find future pregnancies to be just as resistant to treatment. Other options besides pregnancy may be safer choices.
Medication Options:
If your next pregnancy is similar or worse, starting with a specialist like a maternal-fetal-medicine doctor (perinatologist) is helpful to ensure you get the care you need. It can be difficult to change to a new doctor after you get sick, and some clinicians may be uncomfortable or unfamiliar with treating severe HG.
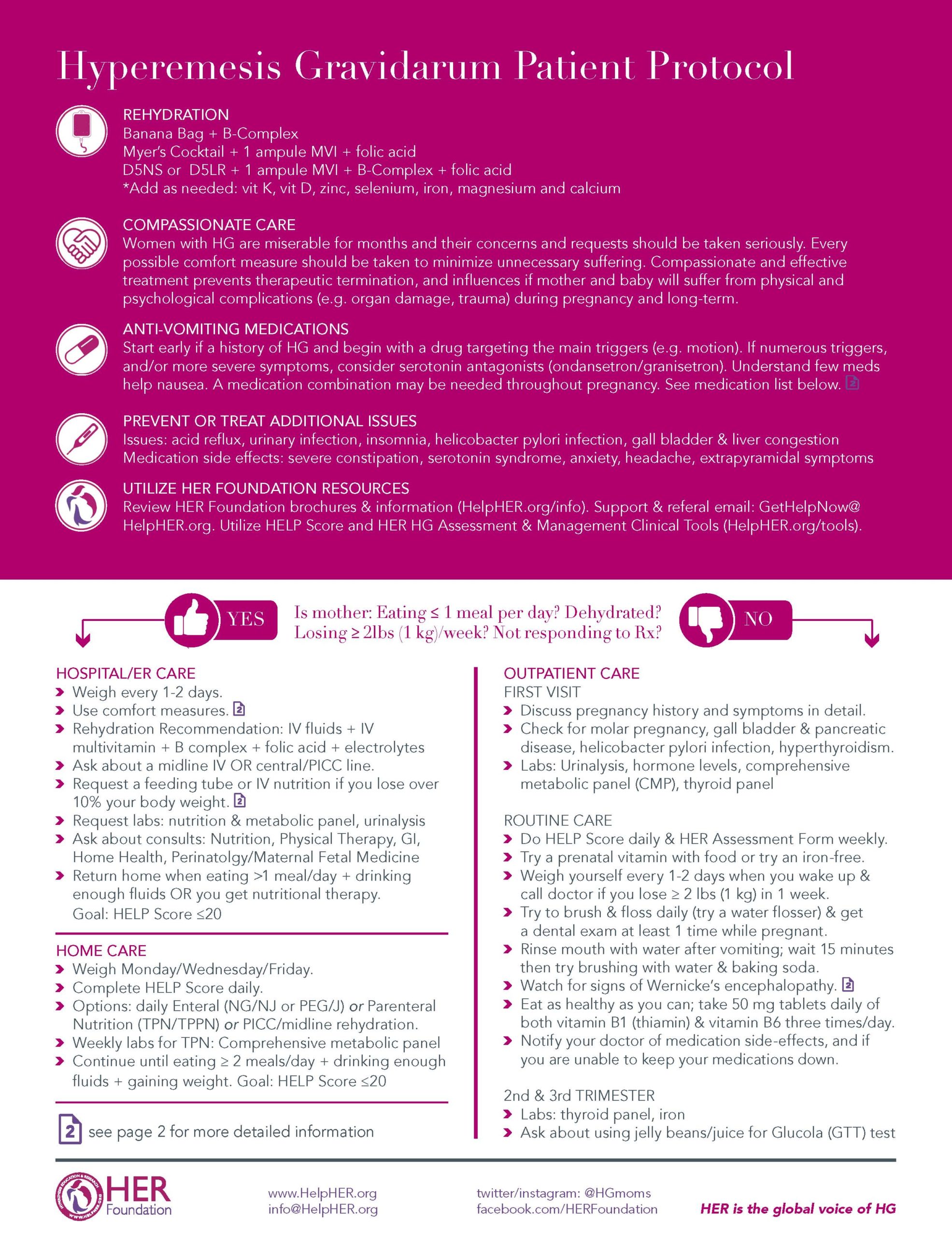
Share the HER Foundation clinical resources with your health care team and discuss the treatment algorithm to see what options you will be offered and when.
Considering most pregnancies are similar if not worse, medication is often necessary to avoid therapeutic termination or miscarriage. Review the medication page on the HER Foundation site to be informed about treatment options. Share treatment resources with your doctor to discuss you options. All medications carry a possible risk, but the risks are often outweighed by the benefits they offer in reducing the symptoms of HG.
Sometimes women require IV nutrition (TPN) which means you will need help at home daily, home health care nurses, and careful monitoring by health care staff to avoid infection and other complications. It is also expensive but can be life-saving. If you are unwilling or unable due to cost, discomfort, or concerns over safety, please read up on it to be informed prior to being sick and know what your insurance will cover. You might experience severe HG and face the choice between losing your baby or IV nutrition.
Medications may pose a small risk to your baby, and introduce the possibility of side-effects or medication interactions. Combining them may be more beneficial, and may be less risky than a Percutaneous Intravenous Central Catheter (PICC) line – a type of IV placed high up on the arm in a large vein. It can remain in place for a month or longer. PICC lines (or other central lines) are risky and not to be taken lightly. For those very ill, a PICC can be life-saving and necessary, however, avoiding them is ideal. If you feel that you will require extensive medical care, remember these present risks that you cannot always control or prevent. Treat early and aggressively utilize strategies like non-oral medications to prevent severe symptoms.
Know that the severity often repeats in future pregnancies. Proactive, aggressive care that is planned in advance is critical to surviving more severe cases of HG. Sometimes each pregnancy will be worse than the previous even with good care. This could be due to the brain becoming more sensitive to the vomiting stimulus, thus making the brain less able to control the vomiting. If you would not terminate again and enter into pregnancy without a plan and knowledgeable health professional, you are taking a significant risk.
This is something that is very important to all pregnancies, but more so for surviving HG, especially if you have children to care for already or get very sick. Women with very high stress levels have higher rates of postpartum depression, and a greater risk of emotional and behavioral disorders in their child.
It will be difficult if not impossible to maintain a normal routine for your children. You may need to depend on family, friends or day care in order to care for your child(ren) during the worst of HG. This can vary from a few weeks to the entire pregnancy. Contrary to popular belief, HG does not usually end at 13 weeks. It often eases by mid-pregnancy, but some symptoms may last until delivery. The longer HG lasts, the greater your fatigue and debility, and the longer your recovery. In a small number of women, symptoms may continue after delivery.
Multiple pregnancies have a higher risk of nausea and vomiting due to the higher level of hormones in their body.
Try to be in the best physical and mental health possible before pregnancy. Some women lose a lot of weight and plan to be about 10 pounds over their normal (healthy for their height) weight at conception, so they have some weight to lose. Taking high quality prenatals and B complex vitamins in the months prior to HG ensures you start pregnancy with adequate nutritional stores. Getting mental health support and treatment for trauma may also help you cope easier in a future pregnancy.
Surviving HG can be expensive if your insurance coverage is limited, you have severe symptoms, become debilitated, experience complications during or after pregnancy, or you lose your income. You can decrease the stress of HG by having extra money available for unexpected expenses. This will also prevent you from having to make choices in your care based on your finances and not your needs.
One month of medications may cost several hundred dollars, and TPN at home costs upwards of $500 per day (USD). Using discount programs by pharmaceutical manufacturers or like GoodRx is helpful to reduce costs. Without insurance, needed treatments may be too expensive, leaving you to suffer unnecessarily. Ensure you have a plan that will cover all possible treatment options and make sure you have waited the required time period for eligibility. Also check to see if HG would be excluded for some reason. It is also very helpful to know the process for seeing a specialist (e.g. if your insurance requires you to get a referral or prior authorization). Be sure that your preferred doctors and hospital are covered by your insurance, or that you have the extra money required to see doctors outside of your network.
Review your finances closely and determine if you could live without all or part of your income, and for how long. There is no guarantee that you will be able to take a leave from work or be able to return quickly. Alternatively, explore medical disability options and ask your health professional what criteria is used to determine when you would be placed on disability. Also, be familiar with your employer's policies on taking a leave of absence or your vacation time. If your HG symptoms are not severe, consider part-time or flex hours.
Finally, know that physical work is practically impossible with HG. If this is part of your job, other options will need consideration. Recovering from HG and a complicated pregnancy can take months, not just weeks. Planning ahead for this is crucial, especially if you have HG beyond mid-pregnancy.
These complications may return in future pregnancies and present significant risks to the baby if not controlled. The risk of harm to you and baby is high if you do not respond to the treatments offered or cannot tolerate the treatments. The more complicated the pregnancy, the more difficult it is to manage, and the higher the probability you will have an early delivery or other adverse event. Make you’re your pregnancy is managed by a maternal-fetal medicine (MFM) specialist.
Some women have long-term health issues due to HG including heart or brain damage, gallbladder disease, extensive damage to teeth, hernias, stomach ulcers, bone loss, depression, and joint damage (esp. jaw - TMJ). Pregnancy and delivery alone present many risks that can be life-threatening. These risks may be too great for you, especially if you have children at home that depend on you. This is something you will need to discuss in depth with your family and medical professionals before deciding. There are other options such as adoption and surrogacy, which are chosen by women with HG who desire to continue their family and avoid HG. It is very important to understand the risks to you and your child so you can make an informed decision.
You will need as much support as possible to endure HG. Without a supportive person around you, it will be difficult to ensure you get the care you need. When you are ill, it's difficult to advocate for yourself. Since many women with HG go on to experience postpartum depression and anxiety due to trauma, it is critical that you have support beyond pregnancy. Physical recovery can take several months, and emotional recovery much longer. If your partner or spouse is not supportive of another pregnancy or had great difficulty coping with previous pregnancies, ensure you have alternate support systems in place and think carefully about your decision. If you become too ill to care for yourself, you will need someone close by to advocate and care for you.
HG is often very traumatic. The thought of enduring it again often creates a great deal of anxiety for women. If you are still suffering from the trauma of HG, professional help is needed to help you prepare for another pregnancy. Some areas have mental health support therapy and groups that specialize in women's health during and after pregnancy. Your OB may be able to offer referrals. Treatments like EMDR and Brainspotting can help heal the trauma.
It is not uncommon for women to feel anxious when trying to conceive, especially knowing that HG lies ahead. Being prepared and informed about managing HG will ease the anxiety.